On Thursday September 12 2024 the Australian Government announced it will deliver aged care reforms to ensure the viability and quality of aged care, and support growing numbers of older Australians choosing to retain their independence and remain in their homes as they age.
The reforms mean self-funded retirees will pay up to an extra $9000.00 per year for residential care, or if receiving care in their own homes, will be required to pay up to 80% of services such as cleaning and gardening and around 50% of costs such as transport t medical appointments.
Another change from July 1 2025 is providers will keep 2% of each new Refundable Accommodation Deposit (RAD) annually. Since aged care homes in Sydney and Melbourne are currently setting RADs at $1 million or more, for people who are in residence for five years, the aged care facility may withhold $100,000 of that deposit when the resident leaves.
The name 'refundable' may need to be changed.
The government states around 1.4 million Australians will benefit from a new Support at Home program by 2035, 'helping them remain independent, in their home and their community for longer'.
$5.6 billion will be invested in a reform package which represents the greatest improvement to aged care in 30 years, and includes these major changes:
- A $4.3 billion investment in Support at Home, to come into effect on 1 July 2025.
- Essential changes to improve the funding, viability, and quality of residential aged care.
- A no worse off principle will provide certainty to people already in aged care and they won't make a greater contribution to their care.
- The treatment of the family home won't change.
- New laws to protect older Australians in aged care, with stronger powers to investigate bad behaviour and civil penalties for breaching standards
The net impact of the changes is a $930 million spend over four years and a $12.6 billion save over the next 11 years, the release states.
The reforms respond to the recommendations of the Aged Care Taskforce, which brought together older Australians, experts and residential aged care providers and recommended that Australians make a reasonable means tested contribution to the cost of their care.
The reforms have received bipartisan support.
The announced details are:
Better support for Australians to age at home
Older Australians increasingly want the freedom, support and choice to remain in the home and community they love. In the past 10 years, the number of Australians in home care has increased fourfold.
To cater to the changing preferences of older Australians, the Albanese Government will invest $4.3 billion in a new system of home care, called Support at Home, which will come into effect on 1 July 2025, and will help Australians remain independent, in their home and their community for longer.
By 2035, Support at Home will help around 1.4 million people stay in their homes as they age.
Support at Home will provide support for:
- Clinical care (e.g. nursing care, occupational therapy)
- Independence (e.g. help with showering, getting dressed or taking medications)
- Everyday living (e.g. cleaning, gardening, shopping or meal preparation)
The Government will pay 100 per cent of clinical care services, with individual contributions going towards independence and everyday living costs.
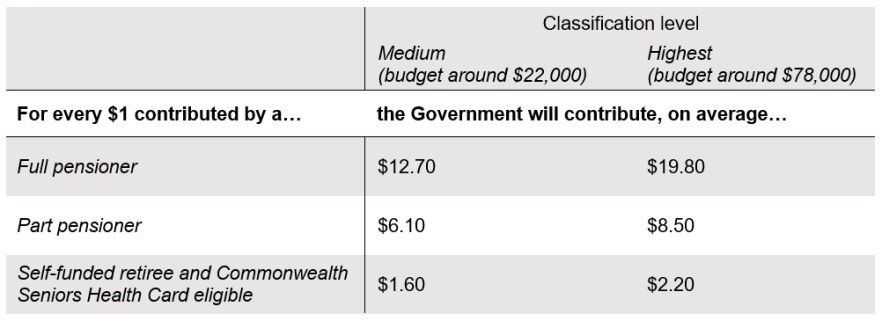
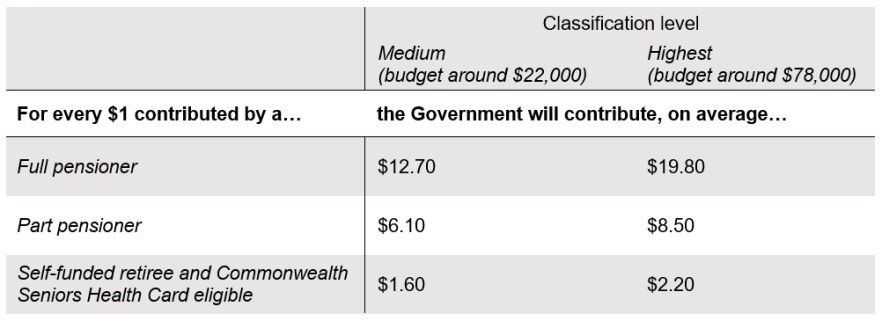
How much someone contributes will be based on the Age Pension means test and highly dependent on their personal circumstances, from the level of support they are assessed to need, to their combination of income and assets.
Click here to see how different Australians would contribute to Support at Home.
A lifetime contribution cap will apply across the aged care system and means no one will contribute more than $130,000 to their non-clinical care costs – whatever their means or duration of care – with every Support at Home contribution counted towards the cap.
The government states some of the benefits of Support at Home include:
- Support for 300,000 more participants in the next 10 years.
- Shorter average wait times from assessment to receive support.
- More tailored support, with 8 ongoing classifications all the way up to around $78,000 a year.
- Support for home modifications, with up to $15,000 to make homes safer.
- Fast access to assistive technology, like walkers and wheelchairs, including a new equipment loan scheme.
Support at Home participants will also have expanded access to restorative support to get back on their feet after an illness or injury, through a 12 week program that works with a team of allied health and other professionals.
According to the Productivity Commission, up to 70 per cent of Australians would prefer to die in the comfort of their own home, but fewer than 10 per cent actually do. Support at Home participants will be eligible for up to $25,000 in additional support to spend their final 3 months at home, so they can be surrounded by loved ones in an environment they cherish, instead of rushing precious moments into hospital visiting hours.
Click here to learn more about Support at Home.
Changes to the funding, viability, and quality of residential care
As the Aged Care Taskforce Report made clear, by 2050 the residential aged care sector will need $56 billion in capital funding to upgrade existing aged care rooms and build the additional rooms that growing numbers of older Australians will need.
In the next 40 years, the number of Australians aged over 65 is expected to more than double, with those aged over 85 to more than triple.
Current funding arrangements are not sufficient: in 2022-23, 46 per cent of providers made a loss from accommodation.
The government states a range of reforms will help ensure residential aged care providers can attract the investment they need to keep current facilities open, improve quality, and build new facilities.
As recommended by the Aged Care Taskforce, these measures include:
- Larger means-tested contributions from new entrants.
- A higher maximum room price that is indexed over time.
- The retention of a portion of refundable accommodation deposits by providers.
The treatment of the family home won't change. Half of new residents will not contribute more under the new consumer contributions:
- All “fully supported” residents will not contribute more.
- 7 in 10 full pensioners will not contribute more.
- 1 in 4 part pensioners will not contribute more.
For every $1 an older Australian contributes to their residential aged care, the Government will contribute an average of $3.30.
The Australian Government’s package of accommodation measures responds to the need to support viability while setting out a pathway to phase out Refundable Accommodation Deposits (RADs) in the longer term.
The details are:
Increasing the maximum accommodation price to $750,000 and indexing over time
Under current arrangements, providers must seek the agreement of the Independent Health and Aged Care Pricing Authority to charge above $550,000 for a room. This has not changed since 2014, despite significant increases in accommodation costs over the past decade.
The government has accepted the Aged Care Taskforce (Taskforce) recommendation to immediately increase this price and index it over time. From 1 January 2025, the government will increase the price requiring approval to $750,000 and index it on 1 July each year to the consumer price index. This is in line with a recommendation of the 2017 Legislated Review of Aged Care (the Tune Review).
This change will reduce red tape for providers and give them greater confidence in developing or updating high quality accommodation. It will also make it easier for providers to plan new builds by giving confidence they can be financially viable projects.
This change will not impact existing residents and there will still be a range of accommodation available at lower prices. Providers will still be able to apply to have room prices above the new maximum.
Refundable Accommodation Deposit Retention to be Introduced
From 1 July 2025, providers will be required to keep a portion of each new RAD, with the amount of retention capped at 5 years to protect residents who remain in care for a long time.
The amount retained would be calculated based on a retention rate of 2% per annum of the RAD balance, with the amount debited monthly. This change would also apply to Refundable Accommodation Contributions (RACs) which are used by residents that receive support for some but not all of their accommodation deposits.
The no worse off principle for existing residents means this change will not apply to the RADs or RACs of residents who enter residential care before 1 July 2025.
However, as an example, and as aged care homes in Sydney and Melbourne are setting RADs at $1 million or even more, this means in the case of people who are in residence for five years, the aged care facility may withhold $100,000 of that deposit when the resident leaves.
Daily Accommodation Payment Indexation to be Introduced
The Daily Accommodation Payment (DAP) that residents pay is currently fixed at the time of entry and this means that over time the value of the accommodation payments residents make to providers reduces in real terms, as the cost of maintaining that accommodation increases. To address this inconsistency, the government will require that the DAPs for all residents entering after 1 July 2025 be indexed.
Under this arrangement, providers will increase the DAP they charge residents twice per year in line with changes in the consumer price index. This is consistent with increases to the government-funded accommodation supplement for supported residents.
This change will not apply to Daily Accommodation Contributions (DACs).
The no worse off principle for existing residents means this change will also not apply to the DAPs of residents who enter residential care before 1 July 2025.
Review of accommodation supplement and accommodation price settings
The government will undertake a review of the accommodation supplement and a number of other accommodation settings over the next 2 years. This review will consider:
- the current rates of accommodation supplement
- incentives for providers to develop and maintain good quality accommodation and
- incentives to accept low means participants.
Viable pathway to phase out RADs in the longer term
Subject to a review of sector readiness in 2030, the Taskforce recommended that the sector be transitioned to not accept new RADs by 2035. The Taskforce noted the concerns raised by the Royal Commission into Aged Care Quality and Safety (Royal Commission) about the sector’s reliance on RADs. However, the Taskforce considered the Royal Commission’s suggested timeframe for phasing out RADs from July 2025 was considered too aggressive and would disrupt the sector, putting service availability for older people at risk.
The Government will commission an independent review of sector readiness in 2029-30, to support consideration of phasing out RADs by 2035.
Read more about how accommodation reform and resident contributions will ensure the growth and viability of residential aged care.
How Different Australians would contribute to their Residential Care
Current state
Everyday living: All residents pay a Basic Daily Fee, set at 85% of the basic age pension ($63.57 per day). The government tops this up with a Hoteling Supplement for all residents of $12.55 per day (as at 20 September).
Care: Residents with sufficient assets and income pay a means tested care fee.
Accommodation: The government funds accommodation in full or part for supported residents - usually full or part pensioners. Non-supported residents may choose to pay with a fully refundable accommodation deposit (RAD) or a daily accommodation payment (DAP).
Future state
Everyday living: No change to Basic Daily Fee. Hoteling Supplement to be means-tested, beginning once a resident has more than $238,000 in assets, $95,400 in annual income, or a combination of the two.
Care: Means-tested care fee abolished and a non-clinical care contribution introduced, with clinical care fully funded by government. Residents begin to pay the new contribution once they have more than $502,981 in assets, more than $131,279 income or a combination of the two. The contribution is capped at $101.16 a day and is paid for the first four years in care. Additionally, once a resident has paid $130,000 in contributions to Support at Home and non-clinical care in residential care they will no longer pay the non-clinical care contribution.
Accommodation: No change to who is eligible for government support with accommodation costs. For residents who choose to pay for their accommodation with a RAD, providers will retain 2% each year for five years, to ensure the quality of facilities is maintained. The treatment of the family home will be unchanged, with only the first $206,039 assessable for means-testing.
No change for existing residents
All residents living in residential aged care before 1 July 2025 will not see a change in their accommodation costs or contributions. Their contribution rates will be preserved and won’t change.
Click here to see how different Australians would contribute to their residential care.

No worse off principle for Australians already in aged care
A no worse off principle will provide certainty to people already in aged care and they won't make a greater contribution to their care.
Support at Home
When Home Care participants transition to Support at Home, from 1 July 2025, they will maintain the same level of funding and retain any unspent funds.
Everyone who, as of 12 September 2024, is receiving a Home Care Package (a package), on the National Priority System, or assessed as eligible for a package, will make the same contributions, or lower, as they would have under Home Care arrangements. They will stay on the existing contribution arrangements when they move to residential care, unless they opt to move to the new program.
Residential aged care
The new contributions and accommodation arrangements will only apply to new entrants to residential aged care from 1 July 2025. Everyone in residential care on 30 June 2025 will maintain their current arrangements until they leave care.
Budget impact
Aged care is one of the biggest pressures on the Budget, the government has stated, and, without action, spending is expected to more than double as a share of GDP over the next 40 years.
The Government currently pays 76 per cent of residential care costs and 95 per cent of home care costs.
The government has stated this package improves aged care and strengthens the Budget at the same time. It is a combination of new investments and new contributions but with generous transitional arrangements.
The net impact of the changes is a $930 million spend over four years and a $12.6 billion save over the next eleven years.
The government states that as a result of the reforms, by 2034-35:
- Annual growth in spending on aged care is expected to moderate. Average annual growth over the decade to 2034-35 was 5.7 per cent at Budget and will come down to 5.2 per cent.
- Aged care spending as a share of GDP is projected to moderate, from 1.5 per cent of GDP to 1.4 per cent, even as the number of participants and the quality of care increase.
Government investment in aged care will continue to grow, year on year, every year, growing more sustainably over time.
Under the reforms, the Government will pay:
- 100 per cent of clinical care costs, regardless of individual means, and
- The majority of aged care costs overall, including:
- 73 per cent of residential care costs and
- 89 per cent of Support at Home costs.
For every $1 an older Australian contributes, the Government will contribute an average of $3.30 to residential care, and $7.80 to Support at Home.
New laws to protect the rights of older Australians
The new Aged Care Act legislation, which will enable the reforms, will soon be introduced to Parliament. It includes:
- A Statement of Rights for older Australians in aged care, with a positive duty for providers to uphold those rights.
- New duties to hold providers and people in positions of leadership accountable, along with a compensation pathway.
- New Quality Standards to drive continuous improvement and high quality care.
- Stronger regulatory powers to protect people from harm.
- New whistleblower protections.
- A regulator with stronger investigative powers.
- A new, independent statutory Complaints Commissioner.
Prime Minister Anthony Albanese stated on Thursday September 12:
“At the heart of my government is a simple principle: putting the “care” back into aged care.
“Older Australians built this country, shaped our economy, did the hard yards. They embody the strength and the spirit of our nation.
“Our government is working to ensure that the aged care system that supports them is stronger now and sustainable into the future.
“Reforms like this do not happen every day. They are once-in-a-generation, and my Government is proud to deliver them, as we said we would.”
Treasurer Jim Chalmers said:
“This is how we Budget for better care. This is how we fund the care Australians need and deserve as they age.
“This is how we improve aged care and strengthen the Budget at the same time.
“These reforms are all about delivering better care for more people in a more sustainable way.
“It’s a step change in care, and a structural reform to the Budget.”
Minister for Aged Care Anika Wells said:
”We’ve heard the message from older Australians: they want support to stay in the homes and communities they love.
“Support at Home will help around 1.4 million older Australians do just that, with shorter wait times, more levels of support, and funding for home modifications.
“The Government will pay 100 per cent of clinical care services, with people contributing towards their support services like help with showering, gardening or meal preparation.
“Older Australians will get support to spend their final weeks at home, surrounded by loved ones in an environment they cherish, instead of rushing precious moments into hospital visiting hours.”
Chief Executive Officer of COTA Australia – the leading advocacy organisation for older people – Patricia Sparrow said that while it took too long to get to this point, the fact that the Aged Care Act has now been introduced is good.
Ms Sparrow also said the government’s significant focus on and investment in Support at Home will be welcomed by older Australians who want greater choice around ageing at home and to see wait times for care at home significantly decreased.
“Now that we’ve finally got past all the roadblocks stopping the introduction of the Aged Care Act, Parliament now needs to ensure that Australians have adequate time to scrutinise the legislation and provide feedback,” Ms Sparrow said.
“There’s no question that when it comes to aged care in Australia business as usual is unacceptable. Ambitious reform is required to fix the current aged care system to meet the needs of our ageing population and increasingly complex aged care needs and the Aged Care Act is central to making this happen.
“Australians of all ages, including older people, now need the opportunity to look into all the detail contained within the 550 pages to ensure that all of its elements are fair, transparent, easy to understand and equitable for all older Australians.
Ms Sparrow said the Aged Care Act is crucial in delivering long awaited rights for older people that put their voices front and centre of the aged care system.
“We need an Aged Care Act that enshrines the rights of older people. While there is still much detail to go through, it appears the Act includes vital measures required to do that including mechanisms for monitoring and enforcing the rights of older people; the introduction of a person-centred, robust and effective complaints system; detail on how rights will be embedded into daily aged care operations; and a shift to supported decision-making becoming the foundation in aged care so there is an assumption that older people can make decisions for themselves.
“The focus on Support at Home is very welcomed. A $4.3billion investment in Support at Home is vital to ensuring Australians can age at home if they want to and should reduce the unacceptable time people currently have to wait for care at home.
‘We need a sustainable aged care system that allows older Australians can access quality care when and where they need it. We need to review the detail of the Aged Care Act in its entirety to make sure that is the case across the board, but the fact that we’ve got to the point where we can investigate that detail is fantastic.
“For too long older Australians, whether due to systemic ageism or other factors, have not been given ownership of their lives when the time comes for them to access aged care. It’s time that changed and this Aged Care Act will go a long way to ensuring that.
“COTA Australia will now focus on analysing the detail, speaking to older people about the detail, and making sure the voice of older people is heard throughout the next phase of the process.”
![]()